Associate Professor Pradermchai Kongkam, MD, is currently working at gastrointestinal endoscopy excellence center, King Chulalongkorn Memorial Hospital, Bangkok, Thailand. He is the current president of the Thai Association for GI Endoscopy (TAGE). He is well known as an expert in endoscopic ultrasound (EUS) with advanced skill of both diagnostic and therapeutic EUS. He has joined many famous international endoscopy meetings worldwide as lecturers, demonstrators, and trainers. He has trained many young Thai and international doctors to be endosongraphers and endoscopists. His present active research include EUS-guided biliary drainage in malignant hilar biliary obstruction, EUS-guided radiofrequency ablation, EUS-guided needle based confocal laser endomicroscopy. In this conference, he will join and share his experience of novel cutting edge EUS technologies with audience.
Combination of endoscopic-ultrasound guided choledochoduodenostomy and gastrojejunostomy resolving combined distal biliary and duodenal obstruction
Endoscopy 2020 Nov 19 doi: 10.1055/a-1294-9399
Patient
A 68-year-old man presented with abdominal pain, jaundice, and weight loss for 1 month. Abdominal computed tomography revealed a periampullary mass measuring 3.5 × 3.5 × 3.2 cm with dilated bile duct
Procedure
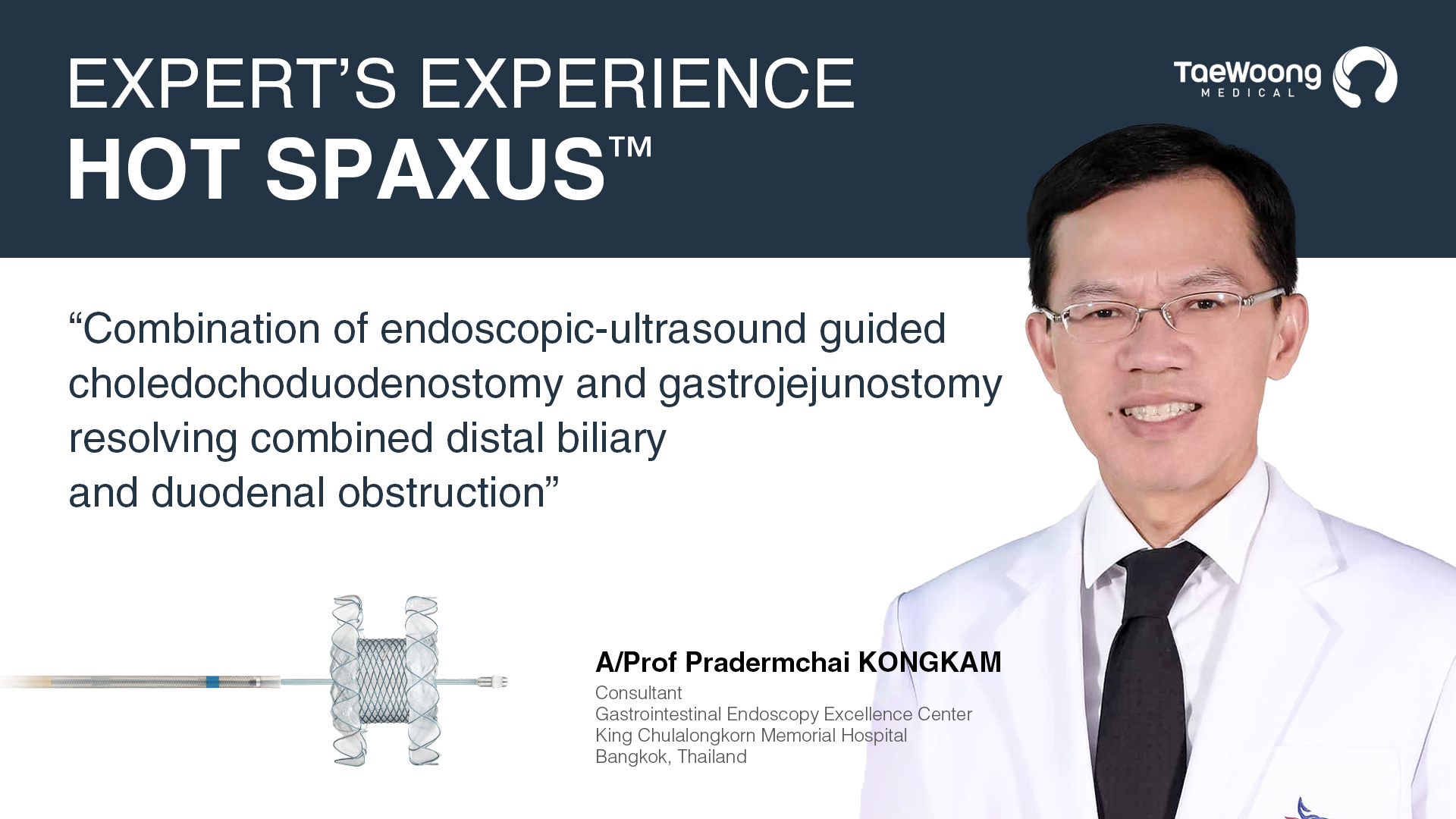
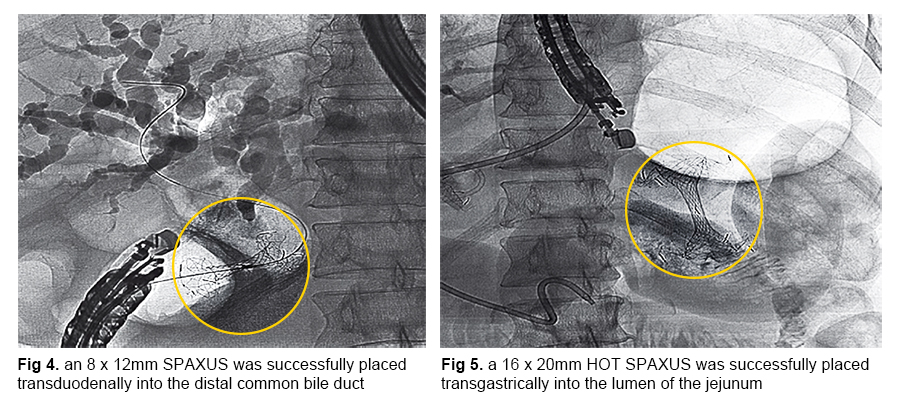
An endoscopic retrograde cholangiopancreatography (ERCP) procedure was not possible owing to a large friable ampullary mass causing supra-ampullary duodenal obstruction. An endoscopic ultrasound-guided choledochoduodenostomy (EUS-CDS) was consequently performed with a linear echoendoscope (GF-UCT180; Olympus, Aizu, Japan). A dilated distal common bile duct (CBD) from an ampullary was shown. A 19-gauge endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) needle with an angled 0.025-inch guidewire was used for puncturing. A 6-Fr cystotome and a 4-mm balloon dilatation catheter (were used for dilation. An 8 × 12-mm lumenapposing metal stent (LAMS) (Niti-S Spaxus; Taewoong Medical Co., Ilsan, Korea) was successfully placed transduodenally into the distal CBD (▶Fig. 4). Subsequently, an EUS-guided gastrojejunostomy was performed. A 10-Fr nasobiliary catheter was placed into the jejunum to flush a mix of diluted contrast, saline, and methylene blue into the lumen of the jejunum in order to distend the small bowel loop. A 16 × 20-mm LAMS with an electrocautery delivery system (Niti-S Spaxus; Taewoong Medical Co.) was successfully placed transgastrically into the lumen of the jejunum (▶Fig. 5). The patient resumed diet with a decline of bilirubin level at 48 hours after the procedure without adverse events.
Please visit to website of Thieme to get the full text of this case report.
