| Dr. Sujievvan Chandran from the Department of Gastroenterology, Austin Health Melbourne in Victoria, Australia discusses his Original Article “Management of pancreatic collections with a novel endoscopically placed fully covered self-expandable metal stent: a national experience (with videos).” |
|
| The purpose of this study was to evaluate a recently developed lumen-apposing, fully covered self-expandable metal stent (FCSEMS) in the management of pancreatic fluid collections (PFCs). The recent literature indicates that endoscopically inserted FCSEMSs may be superior to traditional plastic stenting in the management of PFCs. However, the current literature is limited by small case series undertaken by single operators, across expert centers, and by the use of tubular stents not specifically designed for the management of PFCs. We therefore undertook a multicenter study to address the deficiencies in the current literature. |
|
|
|
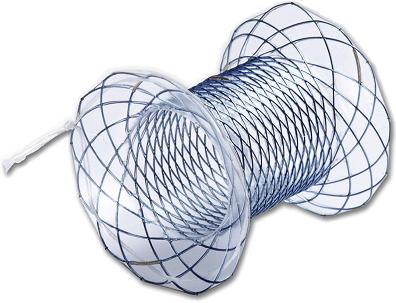
Figure 1. The novel lumen-apposing stent with flared ends to prevent migration and drawstring attachment located at the gastric end to aid extraction |
| We recruited 54 stent cases across 13 centers throughout Australia. Successful insertion occurred in 53/53 (98.1%) with the majority (88.9%, 48/54) being described as easier to insert by the operator in comparison to plastic stenting. This relates to the fact that multiple plastic stenting can be technically more demanding with the associated increased procedural time compared to a single FCSEMS insertion. Stent extraction was also described as superior to plastic stent extraction in the majority of cases (88.6%, 31/35), which can be attributed to the stent design where a draw string at the gastric flange end facilitates rapid collapse and extraction of the stent. The PFC resolution rate in our cohort (76.6%) corresponds to the lower end of what is published in the available literature. We feel that this reflects a real-world experience given the number of centers involved in addition to a larger subgroup of patients with walled of pancreatic necrosis and infected pseudocysts which traditionally have lower resolution rates. Direct endoscopic necrosectomy, while not universally successful across our cohort, did provide a bridge to surgery in a substantial proportion of our patients who were stabilized from a sepsis point of view post FCSEMS insertion which resulted in improvements in the clinical state prior to surgical intervention. Commonly observed adverse events included stent migration (spontaneous and during direct endoscopic necrosectomy [DEN]), recurrent stent occlusion and tissue ingrowth/overgrowth. Stent migration was likely due to the fact that rapid cyst decompression may overcome the anchoring flared ends. Similarly, during DEN the force placed on the stent via the movement of the endoscope overcame the flared end resulting in dis-lodgement into the stomach. Long term stent placement resulted in cases of stent ingrowth related to loss of the silicone coating and overgrowth which indicate that it may not be suitable for the management of PFCs that require long term stenting (eg, disconnected pancreatic tail syndrome). While we have shown a real world experience of PFC management with this novel FCSEMS, randomized control studies are required to further evaluate the benefit of FCSEMS over pigtail stents. Read the abstract for this article online. The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth. |
|